Topics on this page: Overview | FY 2016 President’s Budget for HHS | General Notes | Well-Being of the Nation | Access to Quality Affordable Health Care | Health Care Delivery System Reform for Quality and Economy | Keeping America Healthy | Advancing Science and Research | Serving Americans at Key Stages of Life | Creating a Stronger Department
Overview
ADVANCING THE HEALTH, SAFETY, AND WELL–BEING OF THE NATION
The Department of Health and Human Services enhances the health and well-being of Americans by providing for effective health and human services and by fostering sound, sustained advances in the sciences underlying medicine, public health, and social services.
FY 2016 President’s Budget for HHS
(Dollars in millions)
| 2014 | 2015 | 2016 /1 | |
|---|---|---|---|
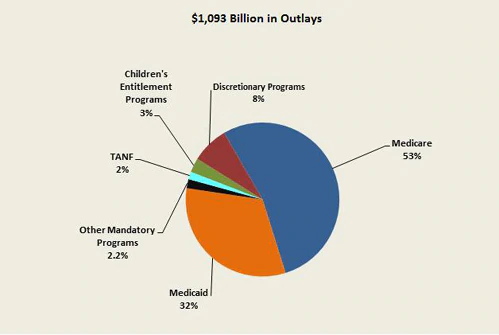
| Budget Authority | 961,166 | 1,048,237 | 1,092,992 |
| Total Outlays | 936,223 | 1,013,051 | 1,093,041 |
| Fulltime Equivalents (FTE) | 74,947 | 77,865 | 80,418 |
Table Footnote
1/ FY 2016 estimates do not include the reductions to mandatory spending that will be applied in FY 2016 as required under the Budget Control Act.
General Notes
Detail in this document may not add to the totals due to rounding. Budget data in this book are presented “comparably” to the FY 2016 Budget since the location of programs may have changed in prior years or be proposed for change in FY 2016. This approach allows increases and decreases in this book to reflect true funding changes.
The FY 2015 and FY 2016 mandatory figures incorporate mandatory proposals reflected in the Budget.
Well-Being of the Nation
The Department of Health and Human Services enhances the health and well-being of Americans by providing for effective health and human services and by fostering sound, sustained advances in the sciences underlying medicine, public health, and social services.
The Budget for the Department of Health and Human Services (HHS) invests in scientific research, health care, disease prevention, early education, social services, and children’s wellbeing, to support healthier families, stronger communities, economic opportunity, and a thriving America.
The President’s fiscal year (FY) 2016 Budget for HHS includes investments needed to support the health and well‑being of the nation, and legislative proposals that taken together would save on net an estimated $249.9 billion over 10 years. An additional $38.4 billion in savings over 10 years to Marketplace subsidies will be realized in the Department of Treasury programs and accounts. The Budget proposes $83.8 billion in discretionary budget authority, an increase of $4.8 billion from FY 2015. With this funding HHS will continue to create opportunities for children and families by ensuring the building blocks for success at every stage of life, promote science and innovation through critical investments, protect the nation’s public health and national security, and focus on the responsible stewardship of taxpayer dollars.
Access to Quality Affordable Health Care
The Affordable Care Act is working to expand health insurance coverage to millions of Americans, including many gaining coverage and access to health care for the first time. The Budget builds on the successes of the Affordable Care Act by extending funding for the Children’s Health Insurance Program, improving and expanding coverage provided to American Indians and Alaska Natives through the Indian Health Service, expanding capacity in the nation’s health centers, making strategic investments in the health care workforce to increase access for rural and underserved populations, and targeting Medicare and Medicaid payments to better support primary and preventive care. The Budget continues to make investments in federal public health and safety net programs to help individuals without coverage get the medical services they need while strengthening local economies.
Expanding Access to Health Insurance Coverage. The Affordable Care Act is making quality, affordable health coverage available to millions of Americans who would otherwise be uninsured through expansion of Medicaid, the Marketplaces, and other private insurance reforms. As a result, the number of uninsured Americans was reduced by about 10 million people in the first year of full Affordable Care Act implementation. As of January 2015, 28 states and the District of Columbia have elected to expand Medicaid to low income adults with household income up to 133 percent of the federal poverty level. The Affordable Care Act is also increasing competition and choice among insurance plans. There are over 25 percent more issuers participating in the Marketplace in 2015 compared to 2014, and about 91 percent of consumers are now able to choose from three or more issuers for their coverage. Additionally, in the first month of open enrollment, 87 percent of consumers got financial assistance to help lower the cost of premiums.
Extending the Children’s Health Insurance Program. The Budget includes an additional four years of funding for the Children’s Health Insurance Program (CHIP) through FY 2019 to align with the maintenance of effort requirement and ensure comprehensive and affordable coverage for children covered by CHIP. This extension will provide stability to state budgets and continuity of coverage to families who rely on CHIP. This proposal is paid for through an increase in tobacco taxes that will help reduce youth smoking and save lives.
Securing IHS Contract Support Costs. The Budget fully funds Contract Support Costs in FY 2016 and proposes to modify the program in FY 2017. In FY 2016, Contract Support Costs will be funded at $718 million, an increase of $55 million over FY 2015. These funds are paid to tribes that administer their own health care programs to cover reasonable costs that the Department did not incur when providing for the direct operation of the program. In FY 2017, the Contract Support Costs program will be reclassified as mandatory providing a long-term approach to fully fund Contract Support Costs and ensuring that tribes receive the support they need to provide health care to their members.
Investing in Health Centers. Health centers are an essential primary care provider for America’s most vulnerable populations. The Budget includes $4.2 billion for health centers, including $2.7 billion in mandatory resources, to serve approximately 28.6 million patients in FY 2016 at more than 9,000 sites in medically underserved communities throughout the country. These resources will support the establishment of 75 new health center sites in areas of the country where they do not currently exist, advance health centers’ efforts provide quality primary health care services, and support on-going efforts to help uninsured patients navigate their insurance options, enroll in affordable coverage, and understand their benefits.
Bolstering the Nation’s Health Workforce. The Budget makes strategic investments in our nation’s health care workforce to ensure rural communities and other underserved populations have access to doctors and other providers. The Budget includes a $14.2 billion investment beginning in FY 2016 to bolster the nation’s health workforce and to improve the delivery of health care across the country.
Extending the National Health Service Corps. National Health Service Corps clinicians serve in medical facilities in high-need areas of the country, including rural areas and federally funded health centers, where access to care is limited and where shortages of health care professionals often persist. The Budget includes $2.6 billion in mandatory resources for the National Health Service Corps for FY 2016 through FY 2020, which is in addition to $287 million in discretionary funding requested for the program. The proposed investment by the Health Resources and Services Administration (HRSA) is projected to support a historically high field strength of over 15,000 providers and to serve the primary care needs of nearly 16 million patients.
Reforming Graduate Medical Education. The focus of the Targeted Support for Graduate Medical Education program will be to support primary and preventive care, in order to advance the Administration’s goals of higher-value health care that reduces long-term costs. Between FY 2016 and FY 2025, the Budget includes $5.3 billion in total mandatory funding for the Targeted Support program, to be distributed through a competitive grant program to teaching hospitals, children’s hospitals, and community-based consortia of teaching hospitals or other health care entities. This investment will support more than 13,000 residents over 10 years.
Promoting Medicaid and Medicare Primary Care. To continue encouraging provider participation in Medicaid, the Budget invests $6.3 billion to extend the enhanced Medicaid reimbursement rate for primary care services through December 31, 2016, expands the program to include additional providers, and targets the funding by excluding emergency department care. The Budget also supports making the temporary 10 percent Medicare primary care incentive payment program permanent in a budget neutral manner to further expand primary care services.
Health Care Delivery System Reform for Quality and Economy
HHS has made tangible progress in helping to lower costs and improve quality and safety across the health care system. Growth rates for total health care expenditures and Medicare are historically low. At the same time, in part due to the Affordable Care Act, substantial reductions to readmissions and harm to patients have also been realized.
Improving the Way Care is Provided. To drive progress on the way care is provided, the Administration is focused on improving the coordination and integration of health care, engaging patients more fully in decision-making, and improving the health of patients – with an emphasis on prevention and wellness. HHS believes that incentivizing the provision of preventive and primary care services will improve the health and well‑being of patients and reduce costs over the long run through avoided hospitalizations and additional office visits. Furthermore, incentivizing and supporting clinicians and providers to deliver care to beneficiaries in the lowest cost and most clinically appropriate setting is a major opportunity for increased efficiency in our healthcare system.
Improving the Way Information is Distributed. The Administration is improving the way information is distributed by working to create transparency of cost and quality information and to bring electronic health information to the point of care. These efforts will enable patients and providers to make the right decisions at the right time to improve health and care. The Centers for Medicare & Medicaid Services (CMS) is making major strides to expand and improve its provider compare websites, which empower consumers with information to make more informed health care decisions, encourage providers to strive for higher levels of quality, and drive overall health system improvement. In September, CMS released the first set of data under Open Payments, a national disclosure program created by the Affordable Care Act that promotes transparency and accountability by making information about financial arrangements between drug and device manufacturers and physicians and teaching hospitals available to the public.
Improved communication can help providers make more informed care decisions and coordinate the care they provide. The adoption and meaningful use of electronic health records was the first step towards achieving interoperability of health systems to improve communication and enhance care coordination for patients. The FY 2016 Budget includes $92 million for activities in support of interoperability and Meaningful Use. The Office of the National Coordinator for Health Information Technology (ONC) will expand the certification program in order to meet the requirements of meaningful use of health IT across the care continuum and including public health. The Budget supports ONC’s efforts to implement the 2015-2020 Federal Health IT Strategic Plan and the National Roadmap to Interoperability. As of November 2014, 428,317 eligible professionals, hospitals, critical access hospitals, and Medicare Advantage organizations have attested as meaningful users of health information technology, accounting for $26.4 billion in incentive payments through the Medicare and Medicaid electronic health records (EHR) incentive program. HHS is on track to meet the performance goal of 450,000 providers receiving incentive payments for demonstrating meaningful use of health IT in 2015.
Improving the Way Providers are Paid. To improve the way providers are paid, the Administration is testing and implementing new payment models that reward value and care coordination – rather than volume and care duplication. The Budget includes proposals targeted at changing provider incentives and payment mechanisms. One of these proposals represents an improvement in physician payment that replaces the recurring threat of payment reductions known as the Sustainable Growth Rate. The Budget would eliminate this payment system and establish annual physician payment updates while creating incentives for physicians and other practitioners to participate in alternative payment models focused on quality and efficiency. It would also streamline value-based incentives for the physicians who remain outside of such models.
Studying Health Insurance. As part of the Administration’s commitment to incorporating evidence and evaluation into policy solutions, the Budget includes $30 million for a new project to examine how changes in health insurance benefit packages impact health care utilization, costs, and outcomes. This project will use the gold standard randomized controlled trial study design to update the Health Insurance Experiment, a groundbreaking trial begun in 1971 that has benefited policymakers for more than forty years. A new effort is needed to rigorously examine how modern health insurance plans can be redesigned to maximize health status and quality, and minimize unnecessary costs. The requested funds will enable HHS to plan and initiate the study using state-of-the-art evaluation methods to answer critical research questions that cannot be directly addressed through other means. The study will inform the development of health care models that work better for families and providers.
Keeping America Healthy
Investing in a Domestic and International Public Health Preparedness Infrastructure. Epidemic threats to national security arise at unpredictable intervals and from unexpected sources. Because these threats do not recognize national borders, the health of people overseas directly affects America’s safety and prosperity, with far-reaching implications for economic security, trade, the stability of foreign governments, and the well-being of U.S. citizens abroad and at home. The Budget includes $975 million for CDC and Assistant Secretary for Preparedness and Response (ASPR) for domestic and international public health preparedness infrastructure, an increase of $22 million above FY 2015, including $12 million for Global Health Security Agenda Implementation, to build the capacity for a country to detect and respond to a potential disease outbreak or public health emergency and prevent the spread of disease across borders.
The Budget also includes $110 million to respond to unanticipated public health emergencies through support for domestic international activities, such as state and local response and emergency staffing, hospital and containment facilities, infection control, laboratory equipment and supplies, data gathering and analysis, countermeasures, and other potential needs in such an incidence. Within the total, there are resources for staff coordination and training, command and control, and other related logistical needs.
Addressing Prescription Drug and Opioid Misuse. The misuse of prescription drugs impacts the lives of millions of Americans across the country. At the same time, it costs the American economy tens of billions of dollars in lost productivity, increased health care, and criminal justice expenses. As part of a new, aggressive, multi-pronged initiative, the Budget includes more than $99 million in new funding this year in targeted efforts to reduce the prevalence and impact of opioid use disorders. These investments, prioritized by the best evidence available and the greatest opportunity for measurable impact, are in addition to a package of policy changes and executive actions that will further drive reforms.
Fighting Prescription Drug and Opioid Misuse, Abuse, and Overdose Death Prevention. The Budget includes $99 million in new investments across HHS to fight misuse and abuse of prescription opioids and heroin, which together take the lives of 20,000 Americans per year. This investment includes a $54 million increase for the Centers for Disease Control and Prevention (CDC). These funds would support grants to all 50 states for improvements to prescription drug monitoring programs, such as interstate interoperability and improved proactive reporting. Grants will also support national-level activities, including patient safety improvements and enhancements in data quality and monitoring with an emphasis on real-time mortality data. CDC will also apply its scientific expertise to identify risk factors for initiating heroin use to best prioritize prevention efforts throughout the Department and develop and track pain management and opioid prescribing quality measures. These funds will also support an evaluation of demonstration programs proposed for FY 2016 administered by the Substance Abuse and Mental Health Services Administration (SAMHSA).
The Budget includes a $35 million increase for SAMHSA to increase access to opioid addiction treatment services, to implement a community- based demonstration to equip first responders with the overdose reversal drug naloxone and education on its use, and to help state substance abuse authorities develop comprehensive prevention approaches through collaboration with state partners and integration of health information technology systems with strategic plans. The Budget includes a $5 million increase for ONC to improve the integration of Prescription Drug Monitoring Programs with health information technology. In addition, a $5 million increase is included within AHRQ to provide a robust review of evidence and evaluation support regarding Medication Assisted Treatment in primary care settings.
Tracking High Prescribers of Prescription Drugs. The Budget proposes to require states to track high prescribers and utilizers of prescription drugs in Medicaid. By requiring states to identify and remediate prescribing and utilization patterns that may indicate abuse or excessive utilization of certain prescription drugs in the Medicaid program, this proposal would improve program integrity, save $710 million over 10 years, and bolster other efforts to reduce abuse of prescription drugs.
Addressing Over Prescription of Psychotropic Medications for Children in Foster Care. The Budget includes $500 million for a new Medicaid demonstration in partnership with the Administration for Children and Families (ACF) to provide performance-based incentive payments to states through Medicaid, coupled with $250 million in mandatory child welfare funding to build provider and systems capacity through a specialized workforce with specific training, screening and assessment tools, coordination between systems, and fidelity monitoring of the evidence-based interventions. This transformational approach will encourage the use of evidence-based screening, assessment, and treatment of trauma and mental health disorders among children and youth in foster care to reduce the over-prescription of psychotropic medications and improve social and emotional outcomes for some of America’s most vulnerable children.
Reducing Abuse of Part-D Drugs. The Budget proposes to establish a program in Medicare Part D to prevent prescription drug abuse by requiring that high-risk beneficiaries only obtain controlled substances from specified providers and pharmacies.
Bringing Mental Health Out of the Shadows. Mental and medical condition comorbidity results in decreased length and quality of life, and increased functional impairment and cost. Patients diagnosed with a serious mental illness die 25 years earlier than other Americans, and they are also among the least likely to seek treatment. The Budget includes an increase of $35 million, a total of $151 million, within SAMHSA for the President’s Now is the Time initiative to make sure students and young adults get treatment for mental health issues. Reaching 750,000 young people per year and training thousands of additional behavioral health professionals and paraprofessionals, this investment represents a substantial step toward bringing mental health out of the shadows. Additional funds will be used to increase workforce capacity across the nation by expanding an existing partnership with HRSA that addresses the number of licensed behavioral health professionals available and by creating a Peer Professionals program to get training for individuals who have lived through their own battle with behavioral health issues to help reach those in need of treatment. In addition, this increase will help change the attitudes of Americans about mental and substance use disorders and their willingness to seek help through a social media campaign and other outreach efforts.
The Budget also proposes the elimination of Medicare’s 190-day lifetime limit on inpatient psychiatric facility services, removing one of the last obstacles to behavioral health parity in the Medicare benefit.
Promoting Upward Mobility. Improving coordination and effectiveness of anti-poverty programs is essential to moving families out of poverty and into the middle class. As part of the Administration’s commitment to achieving economic mobility, the Budget provides $1.5 billion over 5 years in additional competitive funding that will allow up to ten states, localities, or consortia of states and localities, to use funding from up to four block grants to implement evidence-based and promising strategies for helping individuals succeed in the labor market and improving economic mobility, children’s’ outcomes, and the ability of communities to expand opportunity. The Upward Mobility Projects would build on successful safety net programs, like the Supplemental Nutrition Assistance Program, housing assistance, and tax credits, that help families make ends meet and promote children’s health and educational outcomes.
Addressing Viral Hepatitis. Viral hepatitis is the leading cause of liver cancer and the most common reason for liver transplantation in the United States. An estimated 4.4 million Americans are living with chronic hepatitis; most do not know they are infected. In addition to causing substantial morbidity and mortality, viral hepatitis infection has adverse economic consequences. The Budget includes $63 million for CDC’s Viral Hepatitis program, an increase of $32 million over FY 2015 to focus on controlling the emerging epidemic of hepatitis C virus infection in young people, working to eliminate mother-to-child transmission of hepatitis B virus infection, and decreasing premature death resulting from chronic viral hepatitis infection. These priorities are aligned with the HHS Action Plan for the Prevention, Care, and Treatment of Viral Hepatitis.
Improving Tribal Health. The Budget reflects the President’s reaffirmed commitment to ensure tribal members are able to lead healthy and productive lives. The FY 2016 Budget funds IHS at $6.4 billion, an increase of $486 million over FY 2015. The Budget prioritizes providing quality health care services to Indian Country through both the IHS and tribal health care systems. The Budget includes funding for rising health care costs due to medical inflation, population growth, and pay costs for health care providers, ensuring increased levels of health care are provided to American Indians and Alaska Natives. Also, the Budget expands the Purchased/Referred Care program, provides funding for a new program to help IHS and tribal facilities maximize reimbursements from third-party payers, and funds a crucial health information technology project. As in past years, funding is provided for staffing and operating costs for new and replacement health care facilities that expand both IHS and tribal capacity to provide health care services. The Budget also provides funding for collaboration with SAMHSA to fund programs targeted at Native American Youth through the government-wide Generation Indigenous initiative. This funding will allow IHS to expand the successful Methamphetamine and Suicide Prevention initiative to hire providers to work directly with Native Youth.
Improving Health through Improved Care Coordination. People with multiple chronic conditions represent a growing segment of the population and currently comprise over one-quarter of the U.S. population and two-thirds of Medicare beneficiaries. These individuals are at high risk for adverse health outcomes, use more health care services, and have higher rates of disability, poor quality of life and premature death. The FY 2016 Budget includes $12 million for a new initiative by AHRQ to improve the care and quality of life of patients with multiple chronic conditions. This initiative addresses the challenges of a growing high-cost, high-need patient population by developing and evaluating evidence-based tools to improve care coordination.
Advancing Science and Research
Innovative scientific research and technological breakthroughs are vital for the nation to succeed and thrive in the 21st century. The nation depends on science, technology, and innovation to protect the safety and health of the American people and promote sustainable economic growth and job creation. It is also critical to ensure that the nation’s food supply is safe and secure by enhancing domestic and international capacity and establishing standards based on scientific and public health expertise to address today’s complex food safety challenges. The FY 2016 Budget continues strong investments in these areas to ensure that the nation remains at the forefront of new discovery and improves public health.
Supporting Biomedical Research for Real World Applications. As a result of long-term national investments, scientific and technological breakthroughs generated by research supported by the National Institutes of Health (NIH) are behind much of the gains in health and longevity that the nation has enjoyed. For example, deaths from heart disease have been reduced by more than 70 percent from 1950 to 2008, and cancer death rates have been dropping about one percent annually for the past 15 years. The FY 2016 Budget includes $31.3 billion for NIH, an increase of $1 billion over FY 2015, to continue such progress and maintain the nation’s leadership in the life sciences. NIH’s main areas of emphasis for FY 2016 include advancing basic biomedical and behavioral research, translating basic discoveries into applications that improve the health of patients and communities, harnessing data and technology to further benefit health, and preparing a diverse and talented biomedical research workforce. In FY 2016, NIH estimates it will support a total of 35,447 research project grants, including over 10,000 new and competing awards.
Addressing Alzheimer’s Disease. Alzheimer’s disease already afflicts over 5 million Americans and costs the nation approximately $200 billion per year in health costs – and those numbers are projected to rise steadily as the population ages. Recent advances in our understanding of the genetics and biology of Alzheimer’s have identified new potential targets for innovative therapies to slow and ultimately prevent this devastating disease. NIH estimates it will spend $638 million on Alzheimer’s research in FY 2016, an increase of $51 million over FY 2015 to implement the research components of the National Plan to Address Alzheimer’s Disease, a roadmap to assist in meeting the goal to prevent and effectively treat Alzheimer’s by 2025. Recent research has led to more than 25 drugs in clinical trials for Alzheimer’s disease, with many more in the pipeline for human testing.
Combating Bacteria Resistant to Common Antibiotics. As more strains of bacteria become resistant to an ever-larger number of antibiotics, our treatment choices become increasingly limited, expensive, and in some cases, nonexistent. If this problem continues to expand, a wide range of routine medical procedures could pose a significantly higher risk to patients of developing a potentially untreatable, antibiotic-resistant infection. Annually, at least 2 million illnesses and 23,000 deaths are cause by antibiotic-resistant bacteria. The Administration has prioritized scientific and public health efforts to detect, prevent, and control illness and death related to antibiotic-resistant infections, consistent with the recently released National Strategy for Combating Antibiotic-Resistant Bacteria. The FY 2016 Budget includes a total of $993 million, an increase of $491 million across HHS to accelerate progress in these areas. This funding will specifically support research and development and clinical trials of new drug candidates and diagnostic products to ensure the continued availability of effective therapeutics for the treatment of bacterial infections; surveillance activities to detect the emergence of new antibiotic-resistant threats; and prevention efforts to promote best practices on antibiotic use in health care settings.
Securing the Nation’s Food Supply. The burden of foodborne illness is considerable. Every year, 1 out of 6 people in the United States suffers from foodborne illness, more than 100,000 are hospitalized, and thousands die. The economic loss to industry, farmers, and the public from foodborne diseases is estimated to be over $75 billion a year. HHS has helped advance a more modern food safety system that is shifting from reacting to foodborne illness outbreaks, to one that is poised to prevent outbreaks and enhance response activities in coordination with other federal, state, local, and foreign partners. The FY 2016 Budget includes $1.6 billion within the Food and Drug Administration (FDA) and CDC, an increase of $303 million over FY 2015, to support a broad range of food safety activities. These investments will further the Department’s implementation of the Food Safety and Modernization Act by improving surveillance systems; enhancing response and detection; and establishing the framework for an integrated federal, state, and local system; and improving import safety to prevent foodborne illnesses from domestic and international foods and feed.
In addition, the President is seeking broad reorganization authority in the FY 2016 Budget. With this authority, the Administration is proposing to consolidate the Department of Agriculture’s Food Safety Inspection Service and the food safety components of the Food and Drug Administration to create a single new agency within HHS. The new agency would be charged with pursuing a modern, science-based food safety regulatory regime drawing on best practices of both agencies, with strong enforcement and recall mechanisms, expertise in risk assessment, and enforcement and research efforts across all food types based on scientifically supportable assessments of threats to public health. The Budget schedules for these agencies and programs continue to reflect them in their current alignment.
Advancing Countermeasure Development. As new infectious diseases and public health threats emerge, HHS continues to invest in efforts to bolster the nation’s preparedness against chemical, biological, nuclear, and radiological threats. The FY 2016 Budget includes $646 million, an increase of $391 million, for Project BioShield to support procurements and replenishments of new and existing countermeasures and to advance final stage development of new products. To complement these efforts, the Budget also includes $571 million, an increase of $37 million above FY 2015, within CDC to support the Strategic National Stockpile. Strategic procurement, storage, and maintenance of medical countermeasures are necessary to protect lives during a public health emergency. The requested funding level for the Stockpile will enable CDC to replace some expiring countermeasures and maintain the current preparedness levels.
Advancing Precision Medicine. The FY 2016 Budget includes $215 million for a new cross-Department initiative to focus on developing treatments, diagnostics, and prevention strategies tailored to the individual genetic characteristics of each patient, also known as precision medicine. This effort includes $200 million for NIH to launch a national research cohort of a million or more Americans who volunteer to share their genetic information, expand current cancer genomics research, and initiate new studies on how a tumor’s DNA can inform prognosis and treatment choices. FDA will spend $10 million to modernize the regulatory framework to aid the development and use of molecular diagnostics in precision medicine, and ONC will use $5 million in FY 2016 to help develop technology and define standards and certification criteria to enable the exchange of genomic data. The Office for Civil Rights will also work with the participating agencies to ensure that adequate privacy protections are in place to support implementation of this initiative.
Serving Americans at Key Stages of Life
HHS seeks to serve Americans at key stages of life, when many may be at their most vulnerable. Investments that promote the safety, well-being, resilience, and healthy development of our nation’s children and youth will ultimately pay dividends, as the children of today grow into the employees, parents, and leaders of tomorrow. The Budget also makes investments to help older Americans live as independently as possible while maintaining their freedom and dignity.
Early Learning. In the FY 2016, the President calls on Congress to create a continuum of early learning opportunities from birth through age 5 by providing high-quality preschool for every child, guaranteeing quality child care for working families, growing the supply of early learning opportunities for young children, and expanding investments in voluntary, evidence-based home visiting programs.
Child Care Development Fund. The President’s budget makes a historic investment in early childhood education by providing an additional $82 billion over ten years in mandatory funding for the Child Care and Development Fund to ensure that all low-income working families with children ages three or younger have access to quality, affordable child care. This investment will increase the total number of children served to more than 2.6 million, reaching over 1.1 million additional children, and ensuring that the youngest children from the most vulnerable communities are in high quality settings where they are safe and ready to learn. The Budget also provides a $266 million increase in discretionary funding in 2016 to help states implement the policies required by the new bipartisan child care law and improve the safety and quality of care while giving parents the information they need to make good choices about their child care providers. The Budget also includes $100 million for competitive grants to test and evaluate innovative child care models that better meet the needs of working families, including those who work non-traditional hours.
Investing in Head Start. The Budget includes an additional $1.5 billion above FY 2015 to improve the quality of Head Start services and expand access to Early Head Start, including through Early Head Start – Child Care Partnerships. A total of $1.1 billion will ensure that every Head Start program provides services for a full-day and a full-school year, which research shows promotes better outcomes for young children. An additional $150 million will expand access to high-quality early learning programs for infants and toddlers through Early Head Start and Early Head Start – Child Care Partnerships, and $284 million will help programs keep pace with rising costs without diminishing the quality of services.
Expanding Home Visiting. Home Visiting programs have been shown to improve maternal and child health outcomes in the early years, leaving long-lasing, positive impacts on parenting skills, children’s development, and school readiness. The Budget seeks to extend and expand voluntary, evidence-based home visiting services through the Maternal, Infant, and Early Childhood Home Visiting program by providing $500 million in FY 2016, and $15 billion in mandatory funding from FY 2016 to FY 2025.
Retaining Care for Children. The Budget would lift the exclusion of federal funds for comprehensive health care services for Medicaid-enrolled children receiving inpatient psychiatric treatment to ensure provision of essential health services to vulnerable populations.
Promoting Family-Based Care and Reducing the Use of Congregate Care for Children in Foster Care. The Budget includes a proposal to provide additional support and funding to the child welfare system to promote family-based care, and to provide oversight of congregate care. The proposal includes training and resources for foster care parents to provide specialized care to children with complex mental health and behavioral health needs and a new provision to ensure that congregate care is only used when necessary.
Enhancing Prevention and Permanency Services in the Child Welfare System. The Budget proposes to allow additional federal funding for prevention and post-permanency interventions in the child welfare system. A majority of those services must be evidence‑based or evidence‑informed. Providing such services is often key to preventing the removal of a child from his or her family and being placed into foster care, re-entering into foster care after reunification, or disrupting adoptions. This proposal represents a strategic shift of federal investment to the front-end of the service delivery system to prevent removals and foster care placement from the outset.
Supporting Older Adults. In FY 2016, HHS also seeks to make key investments to address the needs of older Americans, many of whom require some level of assistance to continue living independently or semi-independently within their communities. The Budget also enacts common-sense reforms that help to protect older Americans from identity theft.
Supporting Family Caregivers. The FY 2016 Budget provides $15 million for a new Family Support Initiative focused on ensuring the optimal deployment of public and private resources at the state and community level to support family members caring for older adults and/or people with disabilities across the lifespan. Research suggests that informal family care for the elderly is valued at over $500 billion annually, an amount that exceeded total Medicaid expenditures in 2013. Additionally, over 75 percent of people with developmental disabilities rely primarily on family caregivers. The Family Support Initiative will complement the $151 million in funding included in the FY 2016 Budget for Family Caregiver Support Services and spur innovation to support and sustain the largest provider of our nation’s long-term care: families.
In addition, the Budget includes $5 million for Lifespan Respite Care, $3 million more than FY 2015, to provide resources that will allow caregivers to continue care for their loved ones for longer, and thereby allow more care recipients to remain at home and independent for longer periods of time.
Providing Nutrition Assistance for Older Americans. Nutrition Services are a vital support for older Americans nationwide, many of whom are low-income, as meals provided through home delivery or in senior centers allow many older Americans to remain independent and living at home for as long as possible, delaying or preventing the need for more costly institutional services. The FY 2016 Budget includes over $875 in funding for the Administration for Community Living (ACL) Nutrition Services programs, $60 million more than was provided for these programs in FY 2015. Leveraged further by state and local funding, $40 million of this increase will allow states to continue to provide 208 million meals to over 2 million older Americans nation-wide, helping to halt the decline in service levels for the first time since 2010. In addition to these core investments in Nutrition Services, the FY 2016 Budget invests the remaining $20 million in evidence-based innovations to help ensure that future funding for Nutrition Services programs is spent as efficiently as possible to maximize the impact of these funds.
Protecting Seniors from Identity Theft. Protecting seniors from identity theft is a top priority for the Administration. This Budget requests $50 million to support the removal of Social Security Numbers from Medicare cards, so that millions of beneficiaries will no longer have to fear that their personal identification numbers could be used against them due to a lost, stolen or misused Medicare card.
Improving Access to Medicaid Home and Community-Based Services.
The Budget provides states the option to expand eligibility for the Community First Choice and 1915(i) home and community-based state plan options. The Budget also provides states the option to offer full Medicaid eligibility to medically needy individuals who access home and community-based services under the 1915(i) state plan option.
Advancing Comprehensive Medicaid Long-Term Care. The Budget proposes an eight-year pilot program to create a Medicaid comprehensive long-term care state plan option for up to five states. Participating states would be authorized to provide long-term care services across the continuum of care under one authority, creating equal access to home and community-based care and nursing facility care. The Secretary would have the discretion to make these pilots permanent at the end of the eight years. This proposal works to end the institutional bias in long-term care and simplify state administration.
Creating a Stronger Department
The Budget better positions the Department to fulfill its core mission to protect the health of Americans and provide essential human services. Investments in programs and the infrastructures that support them will improve transparency and efficiency across HHS. These improvements will allow HHS to not only meet the challenges of today, but also those of tomorrow.
Investing in Cybersecurity. As cyber threats continue to multiply and become more complex, it is critical for the U.S. government to ensure that its information systems are protected from any potential attacks. In FY 2016, HHS proposes $73 million, $28 million above FY 2015, to manage and provide oversight to the Department’s Cybersecurity Program. This investment is designed to reinforce and protect the Department’s information technology systems against the growing threats within the cyber community. This funding also supports the Department’s ability to quickly respond to evolving security threats and to better support ongoing infrastructure upgrades. The Budget includes funding to support the continued expansion of the Cybersecurity Operations program, enabling the Department to better ascertain the overall security risk to its systems and ensure compliance with requirements of the Federal Information Security Management Act.
Improving Data Access and Innovation. The FY 2016 Budget includes funding to support HHS in its continuous improvement of the efficiency and effectiveness of its operations and the transparency of federal spending.
The Budget includes $10 million to support the implementation of the Digital Accountability and Transparency Act and to formulate new data standards for grants. HHS will assess the impact of those standards on HHS’ financial policies, processes and systems to ultimately improve data quality, reduce compliance costs and reporting burden for grant recipients, and improve overall business practices.
The Budget includes $10 million to create a Digital Service Team within HHS. The Digital Services Team will drive efficiency and effectiveness of the agency’s highest-impact digital services.
The Budget includes $3 million for the HHS IDEA Lab, which will channel talents of the current workforce in an effort to modernize and increase government efficiency. The IDEA Lab will improve HHS services, business practices, and facilitate the mission of the Department.
Reforming Medicare Appeals. To improve the efficiency of the Medicare appeals system and reduce the backlog of appeals awaiting adjudication at the Office of Medicare Hearings and Appeals (OMHA), HHS has developed a comprehensive strategy that involves additional funding, administrative actions, and legislative proposals. The Budget invests new resources at all levels of appeal to increase adjudication capacity and implements new strategies to alleviate the current backlog. The Budget includes $36 million for CMS to engage in discussion with providers to resolve disputes and additional funding for greater participation in Administrative Law Judge Hearings at OMHA. Additionally, the Budget includes $270 million for OMHA, of which $140 million is in budget authority and $130 million is from legislative proposals. OMHA received over 600,000 claims in FY 2013 and close to 1,000,000 claims in FY 2014. The Budget will expand adjudicatory capacity in new field offices in order to address the backlog in the number of appeals and maintain the quality and accuracy of its decisions. The Budget also includes a package of legislative proposals that provide new authority and additional funding to address the backlog.
Strengthening Program Integrity. The FY 2016 Budget continues to make cutting health care fraud, waste, and abuse a top Administration priority. It includes new investments in program integrity totaling $201 million in FY 2016 and $4.6 billion over ten years. These investments include continuing to fund the full Health Care Fraud and Abuse Control discretionary cap adjustment, increasing mandatory Medicaid Integrity Program funding, and providing more funding to recovery auditors to undertake more corrective actions that will help reduce improper payments. In total program integrity investments in the Budget will yield an estimated $21.7 billion in savings to Medicare and Medicaid over ten years. In addition, the Budget supports efforts to monitor and prevent fraud, waste and abuse in the private health insurance market including the Health Insurance Marketplace.
Building Indian Health Service Facilities. The FY 2016 Budget requests an increase of $179 million for Indian Health Service facilities to support construction across Indian Country. The Maintenance & Improvement program, which provides repairs and improvements to currently utilized IHS and tribal facilities, and the Sanitation Facilities Construction program, which builds much needed facilities to deliver potable water and provide waste disposal to American Indian and Alaska Native people, are increased by over $35 million each. The Budget proposes a substantial increase of $100 million for the Health Care Facilities Construction program to decrease the current Health Care Facilities Construction Priorities list backlog. These investments will have a lasting impact on Native communities, ensuring a healthier population.
Protecting Unaccompanied Children. ACF is responsible for ensuring that unaccompanied children who are apprehended by immigration authorities are provided shelter until they can be placed with sponsors, usually parents or other relatives, who assume responsibility for their care while their immigration cases are processed. This past summer, the Administration responded to a significant increase in the number of unaccompanied children who were apprehended on the southwest border, with an aggressive, coordinated federal response focused on providing humanitarian care for the children as well as on stronger deterrence, enforcement, foreign cooperation, and capacity for federal agencies to ensure that our border remains secure. In part as a result of those actions, the number of unaccompanied children apprehended at the border in FY 2015 is below FY 2014 and the number of children referred to ACF is projected to stabilize. To ensure ACF can take custody of all referred children in FY 2016, the Budget includes $948 million in base funding and creates a contingency fund that would trigger additional funds if caseloads exceed levels that could be supported with base funding and any prior-year carryover.