Request for Information - PreventionX
This Request for Information (RFI) falls directly within the framework of Secretary Azar's Value-Based Transformation Initiative, which aims to catalyze the shift towards a health care system focused on rewarding and improving patient outcomes, not only on reimbursement for procedures. Information gathered from the RFI will be used to inform how HHS could catalyze the scaling and deployment of effective prevention strategies into today's social and economic environment.
Issue: Americans suffer from a steadily declining state of personal health, which is the result of a complex set of factors including lifestyle behaviors, environmental cues, access to health and social services, public infrastructure, and others. At the same time, HHS is working to transform our system from one that pays for procedures and diagnoses to one that pays for improved health outcomes, which includes greater focus on delaying or avoiding disease, through both preventative medical and non-medical services. This can only be achieved by taking action so that individuals and communities are empowered to make healthy choices in every aspect of their lives.
The majority of the nation's $3.3 trillion in annual healthcare costs is used for people with chronic and mental health conditions. Healthcare for preventable non-communicable diseases, including heart disease and stroke, type 2 diabetes, kidney disease, and obesity costs the overall US healthcare system over $580 billion annually.1 Increasingly, providers, insurers, and policymakers are focusing on value-based care and outcomes, placing particular emphasis on lowering the incidence of high-cost episodes of care and preventing the progression of highly prevalent chronic conditions where possible.2 Preventing the onset and/or progression of disease ultimately generates the most value for individuals, communities, payers, and society. While there have been some successes, more than 30 million Americans are now living with diabetes, 75 million are hypertensive, and nearly 40% of American adults are obese.3, 4, 5 Despite advances in the development and availability of pharmaceutical treatments for many of these conditions, they have done little to curtail their prevalence among the American population. We have not invested nearly as much in maintaining healthy populations as we have in providing care to the sick. Moreover, effective behavioral interventions have been exceedingly difficult to develop and scale. As a result, we have more effective tools to treat diseases than we do to prevent them. It is time to for us to focus more on transforming prevention--and in doing so, realizing its full value.
Current State: The benefits of a healthy diet and lifestyle are well known but poorly characterized.6 Ample evidence links healthy lifestyle behaviors to a decreased risk for onset of, or adverse health consequences associated with, chronic conditions like type 2 diabetes, obesity, chronic kidney disease and hypertension.7, 8, 9, 10, 11 Yet, relatively few individuals and communities are benefiting from effective, scalable behavior change interventions. Misalignment of incentives in the health system account for some of the current gap between the science of prevention and its implementation. Both public and private payers currently devote considerably fewer resources to prevention than they do to treatment—despite the fact that investments in prevention offer greater potential value, as measured by lower total costs of care and improved health outcomes.
The CDC Three Buckets of Prevention framework categorizes interventions according to three discrete approaches on a continuum of prevention from healthcare to public health.12 Buckets 1 and 2 are patient-oriented and focus on both traditional and innovative clinical prevention approaches. While Bucket 1 focuses primarily on services provided within clinical settings, Bucket 2 begins to bridge the divide between clinical and community services and settings. Bucket 3 completes the transition from clinical to community health orientation by focusing on population-oriented interventions that are intended to protect and improve the health of populations and the community as a whole.
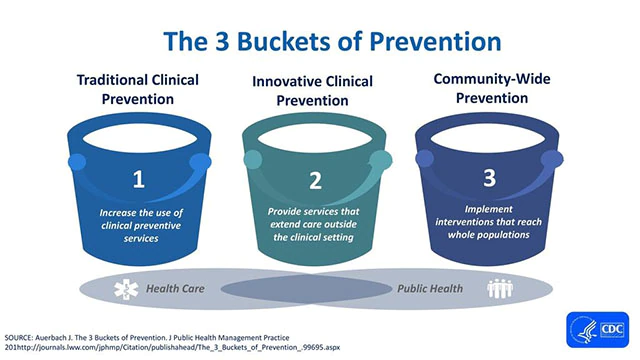
The 3 buckets of prevention.12
American ingenuity, whether manifested through scientific advances, entrepreneurial pursuits, or rapid allocation of capital and resources towards solving problems, has fueled American and global prosperity for centuries. Interventions like those promoted under CDC's 6|18 and HI-5 initiatives present some footholds for innovation, but they are relatively few in number and have proven challenging to effectively scale.13, 14 Moreover, there are few ideas or innovative approaches for effectively bridging the divide between Buckets 2 and 3.
The relative importance of specific barriers to innovation differ across the three buckets. However, the following seven barriers present challenges to scaling disease prevention programs in all three buckets:
(1) No clear efficacy and market validation pathways for prevention strategies such as those that exist for pharmaceuticals (e.g. clinical trial results, FDA approval).
(2) Long iteration cycles, sometimes spanning decades, for developing, testing, and improving disease prevention programs, leading to low levels of innovation that scale beyond local communities.
(3) Failure to appreciate the complexity of behavior change at scale, using methodologies such as human-centered design, choice architecture and other behavior change strategies.
(4) Sparse innovation pipeline, lack of financial incentives for investors to support entrepreneurs, and limited reimbursement incentives from insurers because benefits accrue to a more wide-ranging group of stakeholders
(5) Prevention paradox, where the highest number of cases are made up of low-risk individuals, making it difficult to identify appropriately targeted populations for prevention strategies.
(6) Difficulty to productize prevention strategies, as opposed to pharmaceuticals, which can more easily be distributed around the world with minimal marginal costs and impact on efficacy.
(7) Intra- and Inter-sectoral fragmentation of data, cultures, regulations, and incentives, all of which impede free exchange of ideas and collaborative implementation of new platforms, interventions, and strategies for improving health outcomes.
As a result of these barriers, today there are two co-existing and conflicting realities. The first is driven by emerging technologies, like smartwatches, fitness bands, or other app-based sensors, that have enabled new entrants into a burgeoning consumer-facing disease prevention and health promotion industry. In 2018, nearly $8.1 billion was invested into digital health startups.15 While this reality is characterized by rapid product development cycles, the benefits to public health are still uncertain. Effectively leveraging these new technologies to improve clinical care remains challenging; realizing their potential to improve population health is even more difficult.
The second reality consists of the current public health prevention infrastructure, which relies on using rigorous, evidence-driven research on nutrition, sleep, physical activity, and other behaviors to develop guidelines and programs to promote population health. While these guidelines and programs are often rooted in epidemiological and clinical science, they do not always account for scalable behavior change or adequately address broader social or economic forces that shape health and behaviors. Consequently, guideline adoption, implementation, program uptake, and, most importantly, impact, may be limited. As a result, evolving advancements in science and technology that could improve population health do not translate efficiently into the existing public health infrastructure, and interventions for chronic health conditions often don't fit in with the constraints of everyday living.
Scope and Assumptions
- We are specifically interested in novel interventions for non-communicable diseases, not infectious diseases. While important, infectious diseases that are chronic in nature are not in scope for this initiative.
- For the purposes of this RFI, we are concerned with chronic health conditions, by which we intend to mean common and costly health conditions including but not limited to: hypertension, high cholesterol, type 2 diabetes and prediabetes, obesity, and chronic kidney disease.,
- We are interested in information regarding prevention strategies that align with Buckets 2 & 3 of the Three Buckets of Prevention framework referenced above.
Our Questions
Barriers and Opportunities to Effective Preventative Health
- In your estimation, what have been the most significant barriers to more effective prevention and delayed progression of chronic health conditions in the US?
- What scientific advances are still needed to design, implement, and effectively scale effective Bucket 2 and Bucket 3 prevention interventions for common chronic health conditions?
- How can insights from human-centered design, behavioral science, and systems engineering be better incorporated into design, testing, and validation of Bucket 2 and Bucket 3 interventions?
- Despite extensive evidence suggesting the health benefits of diet and behavior change in preventing chronic health conditions such as obesity and type 2 diabetes, many populations continue to see steady increases in the prevalence of these conditions. Why are more Americans not adopting diet and behavioral changes?
- What evidence-based insights from any domain have the potential to create entirely new classes of interventions in Bucket 2 and Bucket 3?
- What are the key barriers to commercialization of effective prevention products, services, and other strategies with clear public health benefit?
PreventionX Theory of Change
- What are some of the most effective, but not well-publicized prevention strategies (e.g. those found in CDC's 6|18 and HI-5 programs) within Buckets 2 and 3 (or anywhere on the continuum between them)? What has been their key to success? Specifically, we are also interested in interventions that have proven effective on a smaller (e.g., health system or community) scale and are candidates for further testing or expansion.
- How can entrepreneurs and/or technology help drive the development and scaling of prevention strategies that address common chronic conditions?
- What models or methods are available to accelerate the testing, piloting, validation and (if efficacious) scale-up of Bucket 2 and Bucket 3 interventions for common chronic health conditions?
- What datasets, whether clinical, environmental, claims, or other, would, in combination, best spur development of innovative and effective prevention strategies to address common chronic conditions?
- What available metrics and indicators would best measure the efficacy of prevention strategies specific to Buckets 2 and 3?
Public-private Partnerships
- Are you aware of examples of effective public-private partnerships at any scale?
- How can/should public-private partnership models be used to address some of the underlying barriers to scalable prevention strategies?
- What sectors or stakeholders should HHS prioritize for engagement as part of this effort?
Your Response
The period for public comment begins on October 24, 2019. Email your responses to preventionx@hhs.gov, with the subject line "PreventionX RFI Comment" by December 20, 2019.
Respond concisely and in plain language. You may use any structure or layout that presents your information well. You may respond to some or all of our questions, and you can suggest other factors or relevant questions, however please indicate in your response which questions from this RFI you are addressing. You may also include links to online material or interactive presentations. Clearly mark any proprietary information, and place it in its own section or file. Responses are not offers, and they do not create a contract between you and the government. Your response will become government property, and we may publish some of its non-proprietary content.
Helpful References
- Kidney X Innovation Accelerator – A public-private partnership between HHS and the American Society of Nephrology
- The Three Buckets of Prevention--A conceptual population health and prevention framework with 3 categories—or "buckets"—of prevention
- Health Impact in 5 Years (HI-5)--CDC's HI-5 initiative highlights non-clinical, community-wide approaches that have evidence reporting 1) positive health impacts, 2) results within five years, and 3) cost effectiveness and/or cost savings over the lifetime of the population or earlier.
- 6/18 Initiative--CDC's 6|18 Initiative connects healthcare purchasers, payers, and providers with CDC researchers, economists, and policy analysts to find ways to improve health and control costs with the 6|18 interventions
Background on HHS
The U.S. Department of Health & Human Services (HHS) is exploring a number of different approaches that would ultimately accelerate the pace of innovation, scaling, and adoption of prevention strategies.
As a helpful reference for responding to this RFI, here we list some of the many responsibilities and activities across HHS that may play a role towards this effort.
- The Food and Drug Administration (FDA) is responsible for protecting the public health by ensuring the safety, efficacy, and security of human and veterinary drugs, biological products, and medical devices; and by ensuring the safety of our nation's food supply, cosmetics, and products that emit radiation.
- FDA is also responsible for advancing the public health by helping to speed innovations that make medical products more effective, safer, and more affordable and by helping the public get the accurate, science-based information they need to use medical products and foods to maintain and improve their health.
- The Center for Medicaid and CHIP Services (CMCS) operates a variety of programs; Medicaid provides health coverage to low-income people and is one of the largest payers for health care in the United States; the Children's Health Insurance Program (CHIP) provides federal matching funds to states to provide health coverage to children in families with incomes too high to qualify for Medicaid, but who can't afford private coverage; the Basic Health Program (BHP) allows states an option to provide affordable coverage and better continuity of care for people whose income fluctuates above and below Medicaid and CHIP eligibility levels.
- The Centers for Medicare and Medicaid Services (CMS) Innovation Center fosters healthcare transformation by finding new ways to pay for and deliver care that can lower costs and improve care. The Innovation Center identifies, tests and spreads new ways to pay for and deliver better care and better health at reduced costs through improvement for all Americans.
- The Centers for Disease Control & Prevention (CDC) is responsible for detecting and responding to new and emerging health threats, tackling the biggest health problems causing death and disability for Americans, putting science and advanced technology into action to prevent disease, promoting healthy and safe behaviors, communities and environment, developing leaders and training the public health workforce, including disease detectives, taking the health pulse of our nation
- The National Institutes of Health (NIH) aims to foster fundamental creative discoveries, innovative research strategies, and their applications as a basis for ultimately protecting and improving health; to develop, maintain, and renew scientific human and physical resources that will ensure the Nation's capability to prevent disease; and to expand the knowledge base in medical and associated sciences in order to enhance the Nation's economic well-being and ensure a continued high return on the public investment in research.
- The Agency for Healthcare Research and Quality's (AHRQ) mission is to produce evidence to make health care safer, higher quality, more accessible, equitable, and affordable, and to work within the U.S. Department of Health and Human Services and with other partners to make sure that the evidence is understood and used. AHRQ priorities are described.
- The Health Resources and Services Administration (HRSA) is the primary federal agency for improving health care to people who are geographically isolated, economically or medically vulnerable. HRSA programs help those in need of high quality primary health care, people living with HIV/AIDS, pregnant women, and mothers. HRSA also supports the training of health professionals, the distribution of providers to areas where they are needed most and improvements in health care delivery.
- The Indian Health Service (IHS) is responsible for providing federal health services to American Indians and Alaska Natives and to ensure that comprehensive, culturally appropriate personal and public health services are available and accessible to American Indian and Alaska Native people.
References
1. Centers for Disease Control and Prevention. Health and Economic Costs of Chronic Diseases. (2019).
2. Medicare, C. for, Baltimore, M. S. 7500 S. B. & Usa, M. Value Based Programs. (2019). Available at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/value-based-programs/value-based-programs.html. (Accessed: 24th July 2019)
3. Centers for Disease Control and Prevention. National Diabetes Statistics Report. (2017).
4. Merai, R. et al. CDC Grand Rounds: A Public Health Approach to Detect and Control Hypertension. MMWR Morb. Mortal. Wkly. Rep. 65, (2016).
5. Hales, C., Carroll, M., Fryar, C. & Ogden, C. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. NCHS Data Brief 288, (2017).
6. Schulze, M. B., Martínez-González, M. A., Fung, T. T., Lichtenstein, A. H. & Forouhi, N. G. Food based dietary patterns and chronic disease prevention. BMJ 361, k2396 (2018).
7. United States Department of Agriculture. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. (2015).
8. United States Department of Agriculture. 2015-2020 Dietary Guidelines. (2015). Available at: https://health.gov/dietaryguidelines/2015/guidelines/. (Accessed: 1st October 2018)
9. Jessri, M., Lou, W. Y. & L'Abbé, M. R. The 2015 Dietary Guidelines for Americans is associated with a more nutrient-dense diet and a lower risk of obesity. Am. J. Clin. Nutr. 104, 1378–1392 (2016).
10. Carlin, A. et al. A life course examination of the physical environmental determinants of physical activity behaviour: A "Determinants of Diet and Physical Activity" (DEDIPAC) umbrella systematic literature review. PLoS ONE 12, (2017).
11. Mok, A., Khaw, K.-T., Luben, R., Wareham, N. & Brage, S. Physical activity trajectories and mortality: population based cohort study. BMJ 365, l2323 (2019).
12. Auerbach, J. The 3 Buckets of Prevention. J. Public Health Manag. Pract. JPHMP 22, 215–218 (2016).
13. The 6|18 Initiative: Accelerating Evidence into Action | CDC. (2019). Available at: https://www.cdc.gov/sixeighteen/index.html. (Accessed: 24th July 2019)
14. Health Impact in 5 Years | Health System Transformation | AD for Policy | CDC. (2019). Available at: https://www.cdc.gov/policy/hst/hi5/index.html. (Accessed: 24th July 2019)
15. 2018 Year End Funding Report: Is digital health in a bubble? Rock Health Available at: https://rockhealth.com/reports/2018-year-end-funding-report-is-digital-health-in-a-bubble/. (Accessed: 24th July 2019)


