HHS FY 2018 Budget in Brief
Topics on this page: FY 2018 President’s Budget for HHS | General Notes | Putting America's Health First | A Commitment to Fiscal Responsibility - Restoring Trust to Generations of Americans | Reforming the American Health Care System | Protecting the Health and Well-Being of Americans | Delivering Hope and Healing to America | Investing in the Health of America's Future | Responsible Stewardship of Taxpayer Dollars and Redefining the Federal Role
Read the full Budget in Brief
PUTTING AMERICA'S HEALTH FIRST
 FY 2018 President's Budget for HHS
FY 2018 President's Budget for HHS
(Dollars in Millions)
| 2016 | 2017 /1 | 2018 | |
|---|---|---|---|
| Budget Authority | 1,119,166 | 1,126,789 | 1,112,883 |
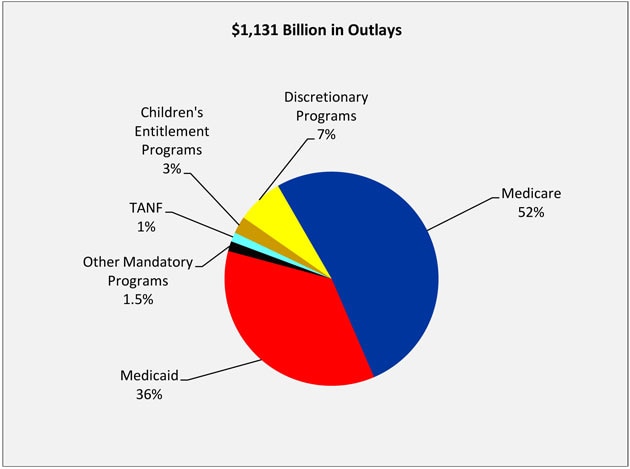
| Total Outlays | 1,103,145 | 1,130,835 | 1,131,256 |
| Full-Time Equivalents (FTE) | 77,499 | 79,505 | 80,027 |
Table Footnotes
1/ A full-year 2017 appropriation was not enacted at the time the budget was prepared; therefore, the budget assumes operations under the Further Continuing Appropriations Act, 2017 (P.L. 114–254). The amounts included for 2017 reflect the annualized level provided by the Continuing Resolution.
General Notes
Detail in this document may not add to the totals due to rounding. Budget data in this book are presented “comparably” to the FY 2018 Budget, since the location of programs may have changed in prior years or be proposed for change in FY 2018. This approach allows increases and decreases in this book to reflect true funding changes. The FY 2017 and FY 2018 mandatory figures reflect current law and mandatory proposals reflected in the Budget.
Putting America's Health First
The Department of Health and Human Services (HHS) is enhancing the health and well-being of the American people by providing effective health and human services and by fostering sound, sustained advances in the sciences underlying medicine, public health, and social services.
The President’s Fiscal Year (FY) 2018 Budget supports the Department’s mission by making strategic investments to protect the health and well-being of Americans; delivering hope and healing to the American people; promoting patient-centered care; strengthen services to tribes; investing in the health of America’s future; and ensuring responsible stewardship of taxpayer dollars for long-term sustainability. Achieving these goals will require HHS to make strategic investments and carry out our mission in the most effective manner possible.
The President’s Budget request for HHS proposes $69 billion in discretionary budget authority and $1,046 billion in mandatory funding to help HHS deliver on the promises the Administration has made to the American people. The Budget focuses resources on direct services and proven investments while streamlining or eliminating programs that are duplicative or have limited impact. The Department’s approach to budgeting this fiscal year puts the American people first by supporting fiscal discipline within the Federal Government and saving taxpayers a net estimated $665 billion over 10 years.
A Commitment to Fiscal Responsibility - Restoring Trust to Generations of Americans
The FY 2018 President’s Budget brings Federal spending under control and returns the Federal budget to balance within ten years. Of its total net estimated ten-year savings over this period, the HHS Budget contributes $665 billion in mandatory savings primarily from giving States new flexibilities to operate their Medicaid programs under per capita caps or block grants beginning in Fiscal Year 2020. The President has embraced these bold reforms that save, strengthen, and secure the promises of the Federal Government’s major benefits programs. The Budget ensures that Medicaid and other programs focus on the most vulnerable Americans that they were intended to serve—the elderly, people with disabilities, children, and pregnant women.
Failing to tackle unsustainable deficit spending means passing growing debt on to our children and grandchildren and creating serious economic damage. The Federal Government’s deficit spending has created a growing debt that cannot be sustained, because it is consuming an increasing portion of national income and limiting resources for private investment and public programs. Over the next ten years, interest payments on our national debt are projected to consume trillions of dollars and surpass annual spending on national defense, Medicaid, or science.
Without action, future generations of Americans will be burdened with unsustainable debt. To restore the people’s trust, we must take a fiscally sustainable approach. The Budget begins the process of expanding choices for individuals and families; enabling market forces and competition to encourage innovation and restrain costs; encouraging self-sufficiency; and promoting federalism, allowing States and localities the flexibility they need to serve their populations.
With responsibility for the major drivers of mandatory spending in the Budget, HHS is in a unique position to help lead the Administration’s efforts to rebuild fiscal solvency and to secure the trust of current and future generations of Americans.
Reforming the American Health Care System
Providing Relief from Obamacare
The Budget includes $250 billion in net deficit savings over 10 years associated with health care reform as part of the Administration’s commitment to expand choices, increase access, and lower premiums. The Administration continues to support a repeal and replace approach that improves Medicaid's sustainability and targets resources to those most in need, eliminates Obamacare’s onerous taxes and mandates, provides funding for States to stabilize markets and ensure a smooth transition away from Obamacare, and helps Americans purchase the coverage they want through the use of tax credits and expanded Health Savings Accounts. The Administration urges the Congress to continue its work to repeal and replace Obamacare. The $250 billion in combined savings accrue to both Treasury and HHS.
The Administration will continue to work with Congress to provide for a stable transition from the burdensome requirements of Obamacare to a health care system that provides Americans with access to care that meets their needs and increases options for patients and providers. The Administration also supports State flexibility to create a free and open health care market and will empower States to make decisions that work best for their markets. In light of these goals, the Budget promotes efficient operations and funds critical activities to continue to operate the law’s health insurance Exchanges.
Reforming Medicaid
The Budget fulfills the President’s pledge to give States the resources and flexibility they need to care for the most vulnerable in their communities through Medicaid. To this end, the Budget reforms Medicaid funding to States starting in FY 2020 through either a per capita cap or a block grant. The Budget also provides other flexibilities to States and encourages them to innovate and test new ideas that will improve access to care and health outcomes. These proposals will save $610 billion through FY 2027 and will allow States to prioritize Federal resources for the most vulnerable populations.
The Budget extends the Children’s Health Insurance Program for two years (through FY 2019) and makes modest reforms that taken together save a net $5.8 billion over the Budget window. The reforms to the Children’s Health Insurance Program ensure the program’s focus on serving the most vulnerable low-income families.
Modernizing the Medical Liability System
The current medical liability system disproportionately benefits a relatively small group of plaintiffs and trial lawyers at the expense of adding significantly to the cost of health care for every American and imposing a significant burden on health care providers. The current medical liability system does not work for patients or providers, nor does it promote high-quality, evidence-based care. The Budget proposes medical liability reforms that will save HHS programs $31.8 billion over 10 years and $55 billion to the Federal Government overall. A significant portion of these savings are attributable to the estimated reduction in unnecessary services and curbing the practice of defensive medicine. These medical liability reforms will benefit all Americans by cutting unnecessary health care spending.
In addition to reducing health care costs, these reforms will help physicians focus on patients and on evidence-based medicine rather than on frivolous lawsuits. By providing a safe harbor based on clinical guidelines, physicians can focus on delivering effective care, and - if an inherently risky medical procedure does not work out as intended - physicians will be able to express sympathy to a grieving family without fear of giving rise to a lawsuit.
Specifically, the Budget proposes the following medical liability reforms:
- Capping awards for noneconomic damages at $250,000 indexed to inflation;
- Providing safe harbors for providers based on clinical standards;
- Authorizing the Secretary to provide guidance to States to create expert panels and administrative health care tribunals;
- Allowing evidence of a claimants’ income from other sources such as workers compensation and auto insurance to be introduced at trial;
- Providing for a three-year statute of limitations;
- Allowing courts to modify attorney's fee arrangements;
- Establishing a fair-share rule to replace the current rule of joint and several liability;
- Excluding provider expressions of regret or apology from evidence; and
- Requiring courts to honor a request by either party to pay damages in periodic payments for any award equaling or exceeding $50,000.
Enhancing Direct-to-Patient Relationships
HHS is committed to reducing regulatory burdens facing medical professionals, especially those serving in rural areas. To achieve this goal, HHS continues to look for ways to improve or eliminate regulations that impede the ability of medical professionals to provide the best possible care to their patients. HHS also believes that health care providers are a valuable resource whose input and ideas are essential to a positive health care reform effort. HHS also is committed to an open and transparent process for developing new voluntary payment models that providers can participate in. Finally, HHS has established various avenues of technical assistance to help clinicians be successful in providing efficient, high-quality care to their patients.
Achieving the President’s goals to reform Medicaid will require providing States with more flexibility to improve healthcare delivery to meet the needs of their unique populations. Direct Primary Care practices, in which physicians offer primary care services to patients at a set price, generally without payer or insurer involvement, are a mechanism to improve physician-patient relationships. Some State Medicaid programs are already testing this innovative care delivery model. HHS will explore opportunities for States and providers to further expand Direct Primary Care, which will support improved health outcomes for Medicaid populations.
Protecting the Health and Well-Being of Americans
Supporting Life-Saving Preparedness and Response Activities
The Department fills a unique Federal role in emergency preparedness and response. HHS is the Federal Government’s lead agency in responding to public health emergencies. The Department coordinates the prevention of, preparation for, and response to public health emergencies and disasters. It supports numerous critical activities to enhance the Federal, State, and local capacity to respond to public health disasters—from outbreaks of infectious disease to chemical, biological, radiological, nuclear, and cyber threats.
The Budget provides $2.9 billion to ensure that the Department is equipped to support life-saving preparedness and response activities aimed at addressing public health disasters and threats. This includes maintaining key investments in biodefense capabilities.
Emergency preparedness initiatives to address pandemic influenza, as well as the research and development of medical countermeasures, are described in greater detail below.
Pandemic Influenza
The Budget supports activities within the Public Health and Social Services Emergency fund to respond to and protect the American people from pandemic influenza threats, such as the H7N9 virus circulating in China. These activities include maintenance of the current stockpiles of vaccines as well as sustaining domestic vaccine manufacturing infrastructure.
Human infections with a new avian influenza (H7N9) virus were first reported internationally in China in March 2013. The World Health Organization has reported 566 human infections with the H7N9 virus during the fifth epidemic, making it the largest to date. This count brings the cumulative number of H7N9 cases reported by the World Health Organization to 1,364.
The FY 2018 Budget includes a $207 million investment to respond to the needs of the American people in the event of an influenza pandemic.
Research and Development of Medical Countermeasures
The Budget invests $1.02 billion into the research and development of medical countermeasures needed during disasters. Using these funds, the Department partners with industry leaders to develop an effective response capability to protect Americans from radiological, nuclear, chemical, and biological threats. The Department supports a broad portfolio of countermeasures to bridge the gap from early discovery to advanced development and procurement. These investments meet a unique Federal role to partner with industry in developing drugs and other countermeasures for which a sufficient market is lacking.
Preparedness Grants
The Budget restructures HHS preparedness grants to direct resources to States with the greatest need and innovative approaches. The Budget will introduce competition, risk, and link awards to performance across ASPR’s Hospital Preparedness Program and CDC’s Public Health and Emergency Preparedness Program. The grants will support entities that are most innovative in their approach to health care delivery system readiness and public health preparedness.
Delivering Hope and Healing to America
The opioid epidemic is the deadliest drug epidemic in American history. Deaths from opioid overdose have risen steadily over the past two decades and have become the leading cause of death from injury in the United States, claiming 91 lives every day. We are losing more Americans to overdoses every year than we did during the entire Vietnam War.
The Administration has made combating opioid abuse and fighting addiction an Administration-wide effort and priority, and the Budget reflects this commitment. It continues to invest in activities to fight opioid abuse, maintains funding for substance abuse treatment, and seeks to improve prescribing practices and the use of medication-assisted treatment.
The Budget also invests in high-priority mental health initiatives by targeting resources for serious mental illness, suicide prevention, homelessness prevention, and children’s mental health.
Improving Prescribing Practices and Expanding Use of Medication-Assisted Treatment
To fight against opioid abuse, medication must be correctly prescribed and utilized. HHS is focused on providing support for cutting-edge research on pain addiction and strengthening our understanding of the epidemic through health surveillance. In addition, the Budget makes investments to improve access to treatment and recovery services, target the availability and distribution of overdose-reversing drugs, and advance better practices for pain management.
Improving Access to Treatment and Recovery Services
Medication-assisted treatment is a proven effective intervention for individuals suffering from addiction. The Budget includes $500 million for the Substance Abuse and Mental Health Administration’s State Targeted Response to the Opioid Crisis Grants authorized in the 21st Century Cures Act to expand access to life-saving, transformative treatments, including Medication-Assisted Treatment. The Budget also continues the $1.9 billion Substance Abuse Block Grant, which States can use to provide life-saving treatments, and $25 million in SAMHSA for other targeted efforts focused specifically on expanding access to critical interventions.
Targeting Availability and Distribution of Overdose-Reversing Drugs
First responders to an overdose in progress have precious little time to save a life by reversing the effects of an overdose. The FY 2018 Budget for SAMHSA includes $24 million to equip first responders with overdose reversing drugs and to train them on their use, supporting the implementation of key provisions of the Comprehensive Addiction and Recovery Act.
Advancing Better Practices for Pain Management
While actions to address prescription opioid abuse must focus on both prescribers and high-risk patients, prescribers are the first line of defense for preventing inappropriate access. The FY 2018 CDC Budget includes $75.4 million to improve the way opioids are prescribed through clinical practice guidelines and support State programs, which help health care providers offer safer, more effective treatments while reducing opioid-related abuse and overdose. CDC aims to save lives and prevent prescription opioid overdoses by equipping providers with the knowledge, tools, and guidance they need.
In addition, the Centers for Medicare and Medicaid Services’ Budget continues to support the agency’s work to implement more effective, patient-centered strategies to reduce the risk of opioid use disorders, overdoses, inappropriate prescribing, and drug diversion.
Improving Access to Mental Health Treatment
In 2015, an estimated 10 million American adults battled serious mental illness, such as a psychotic or serious mood or anxiety disorder. The Budget includes high-priority mental health funding that addresses suicide prevention, homelessness prevention, and children’s mental health. It also includes funding to address the needs of adults with serious mental illness and children experiencing a mental health crisis. The Budget provides $119 million for the Children’s Mental Health Services program, which helps States, Tribes, and communities deliver evidence-based services and support for children and youth with serious mental health concerns. These funds facilitate effective collaboration between child and youth-serving systems such as juvenile justice, child welfare, and education. The Budget also proposes that up to 10 percent of the funds will be available for a new demonstration project focused on earlier interventions. This new set-aside reflects recent research by the National Institute on Mental Health indicating that earlier psychosocial interventions with those who are high-risk may prevent the further development of serious emotional disturbances and ultimately serious mental illness.
The Budget maintains $60 million in critical funding for grants to States, colleges, and the suicide prevention resource center to raise suicide awareness and disseminate best practices for prevention. The Budget also continues to provide funding for the National Suicide Prevention Lifeline, which coordinates a national network of crisis centers by providing suicide prevention and crisis intervention services. Those seeking help can reach the Lifeline at 1-800-273-TALK at any time, day or night.
Providing Patient-Centered Care
HHS is committed to addressing the challenges many Americans continue to confront under a health care system that is failing to meet their needs. The Department is supporting a patient-centered health care reform effort that is aimed at empowering patients, families, and doctors when it comes to making health care decisions. HHS is making progress toward this priority by taking administrative and regulatory actions that will provide the American people relief from the current law, build a partnership with states to improve health care choices for patients, reform the medical liability system, and enhance the doctor-patient relationship. In FY 2018, the Department will invest nearly $400 million in services, training for medical professionals, and approaches that respond to the diverse health care needs across America.
Strengthening Services to Tribes
HHS is committed to providing quality health care to over 2.2 million American Indian and Alaska Native people by effectively leveraging resources and implementing new and innovative ways to improve access to and the delivery of quality health care. As part of the unique government-to-government relationship between the Federal Government and Tribal Governments, the Indian Health Service provides health care to members of more than 567 Federally-recognized tribes. The FY 2018 IHS Budget prioritizes funding for direct health care services, including behavioral health services.
Prioritizing Direct Health Services in Indian Country
The Budget reflects HHS’s high-priority commitment to Indian Country and protects direct health care investments. In FY 2018, the Budget maintains funding for clinical services at $3.3 billion, which includes inpatient and outpatient care in hospitals and clinics, behavioral health services, and dental health services. In FY 2018, IHS estimates that they will serve 2.2 million American Indians and Alaska Natives.
Investing in the Health of America's Future
The percentage of children with obesity in the United States has more than tripled since the 1970s. Today, nearly 20 percent of school-aged children are obese. Children with obesity are at higher risk for having other chronic health conditions and diseases that impact physical health, such as asthma, sleep apnea, bone and joint problems, type 2 diabetes, and risk factors for heart disease.
The Budget represents a commitment to uplifting the health of the next generation by investing in services that promote healthy eating and physical activity. To accomplish this priority, the Budget invests in a new CDC block grant to address childhood obesity and other state priorities, and enhances Children’s Health Insurance Program flexibility.
CDC Childhood Obesity and America’s Health Block Grant
The FY 2018 Budget will support investments in the most effective childhood obesity prevention and intervention strategies within CDC and promote better nutrition, increased physical activity, and prevention of future chronic illness. CDC will continue to provide funding to States to implement programs intended to reduce the risk factors associated with childhood obesity, manage chronic conditions in schools, and promote the well-being and healthy development of all children and youth.
The Budget includes a new CDC $500 million America’s Health Block Grant to increase State flexibility and focus on leading public health challenges. The newly-established block grant will provide flexibility in FY 2018 for each State to implement specific interventions that address its population’s unique public health issues, including interventions to spur improvements in physical activity and the nutrition of children and adolescents.
Responsible Stewardship of Taxpayer Dollars and Redefining the Federal Role
The Budget allows HHS to continue to support priority activities at an overall lower level while restoring fiscal discipline and promoting long-term fiscal stability across the Federal Government. In order to make targeted, strategic investments and carry out the Department’s mission in the most efficient manner possible, the Budget proposes reorganizations and specific HHS efficiencies, proposals to revisit key partnerships within the private sector, and proposals to strengthen the integrity of the Medicare and Medicaid programs.
Reorganizations and HHS-Specific Efficiencies
While large-scale reorganization, workforce restructuring, and efficiency proposals are under development within the Department, the Budget offers select HHS restructuring and efficiency proposals.
Medicare Appeals
HHS remains committed to working with Congress on comprehensive and common sense reforms to the Medicare appeals process. The Budget includes investing $1.3 billion over ten years to address the pending backlog and HHS is pursuing reforms to revamp the process to address appeals as early as possible and prevent escalation to subsequent levels. These changes will make the appeals system easier to navigate, increase adjudicatory capacity to address incoming annual receipts, and reduce backlogged appeals pending at the Office of Medicare Hearings and Appeals and the Departmental Appeals Board. The Department is committed to work with Congress to address the Medicare appeals backlog.
National Institutes of Health (NIH) Structural Changes
NIH will continue to support core mission-critical activities in the Budget, while implementing policies to reduce burden on its grantees. On average, from FY 1994 to FY 2014, NIH spent approximately 30 percent of its research resources on indirect costs, leaving only 70 percent for direct research and other supporting research activities. Other entities, including private foundations and payers, spend a much higher portion of their grants on direct science. The current indirect rate setting process requires each grantee to provide hundreds of pages of documentation to negotiate their indirect rate with the Government.
NIH will implement reforms to release grantees from the costly and time-consuming indirect rate setting process and reporting requirements. Applying a uniform indirect cost rate to all grants mitigates the risk for fraud and abuse because it can be simply and uniformly applied to grantees.
The Budget includes this critical reform to reduce indirect costs and preserve more funding for direct science.
The Budget also proposes the elimination of the Fogarty International Center, but retains all Federal staff and maintains key activities in other NIH Institutes and Centers. This change will enable NIH to focus on higher priority activities.
The Budget consolidates the Agency for Healthcare Research and Quality into NIH and maintains $272 million in discretionary funding for these activities. As part of this consolidation, NIH will conduct a review of health services research across NIH and develop a strategy to ensure that the highest priority health services research is conducted and made available across the Federal Government. The consolidation proposal preserves key activities, such as patient safety research, that improve the quality and safety of American health care. The Budget reduces or eliminates lower-priority programs that overlap with activities administered by other components of HHS.
Revisiting Key Partnerships with the Private Sector
The Budget envisions a recalibration of how to pay for the Food and Drug Administration’s (FDA) premarket review activities. Industry fees are increased to fund 100 percent of costs for premarket review and approval activities in the animal drug, animal generic, prescription and generic drug, biosimilar, and medical device programs. In a constrained budget environment, industries that directly benefit from FDA’s administrative actions can and should pay to support FDA’s capacity. The fee-funded approach is consistent with the overarching goals of the Administration’s Budget, which are to reprioritize Federal spending to advance the safety and security of the American people. The Budget also includes reforms that balance the demand for scientific rigor and access to reliable, life-saving cures. In addition, the Budget will include regulatory relief to the industry and speed the development of safe and effective medical products.
The Budget allows FDA to remain an acknowledged leader among the world’s regulatory agencies in both the number of new drugs approved each year and in the timeliness of review. These proposals will allow FDA to continue carrying out its statutory responsibilities of protecting public health by promoting innovative, safe treatments that are responsive to the needs of the American people.
Strengthening the Integrity of Medicare and Medicaid
The Budget strengthens the integrity and sustainability of Medicare and Medicaid by investing an additional $70 million in new Health Care Fraud and Abuse Control Program funding in FY 2018, targeting activities that prevent fraud, waste, and abuse and promote quality, patient-centered health care.
The increase in funding reflects the Administration’s commitment to fighting fraud and the belief that this investment will pay off in significant returns to the Medicare Trust Fund and the Treasury. For example, recent reports to Congress show Medicare program integrity efforts yielding approximately a $12 to $1 return and law enforcement and litigation efforts yielding a $5 to $1 return.
HHS Operating Plans
Office of the Secretary
- General Departmental Management
- Office for Civil Rights (OCR)
- Office of Inspector General (OIG)
- Office of Medicare Hearings and Appeals (OMHA)
- Public Health and Social Services Emergency Fund (PHSSEF)
- Office of the National Coordinator for Health Information Technology (ONC)
Operating Divisions
- Administration for Children and Families (ACF)
- Administration for Community Living (ACL)
- Administration for Healthcare Research and Quality (AHRQ)
- Centers for Disease Control and Prevention (CDC)
- Centers for Medicare and Medicaid Services (CMS)
- U.S. Food and Drug Administration (FDA)
- Health Resources and Services Administration (HRSA)
- National Institutes of Health (NIH)
- Substance Abuse and Mental Health Services (SAMHSA)